AI and the Evolution of Clinical Documentation: Focusing on Individual Progress Notes
The integration of Artificial Intelligence (AI) in healthcare has been one of the most significant advancements in modern medicine, particularly in the realm of clinical documentation. This technology’s pivotal role extends into various therapeutic areas, simplifying and refining the process of generating detailed progress notes for individual sessions. AutoNotes, an advanced AI-driven platform, is at the forefront of this innovation, offering specialized features for creating precise and efficient individual progress notes for healthcare professionals.
The Importance of Accurate Clinical Documentation
Clinical documentation in individual sessions, whether in mental health, physical therapy, or occupational therapy, is vital for several reasons. It ensures continuity of care, aids in treatment planning, supports legal and ethical record-keeping, facilitates billing, and provides a basis for clinical research. However, the intricacy of individual sessions, which often involve detailed patient reactions and therapeutic interventions, poses unique challenges in documentation. Clinicians must capture comprehensive patient data and progress assessments, all while maintaining engagement with the patient.
AutoNotes: Revolutionizing Progress Note Documentation
AutoNotes has emerged as a crucial tool for clinicians across various therapeutic disciplines, enhancing the documentation of individual sessions. The platform supports various documentation formats like SOAP (Subjective, Objective, Assessment, and Plan), DAP (Data, Assessment, and Plan), BIRP (Behavior, Intervention, Response, and Plan), GIRP (Goal, Intervention, Response, and Plan), SIRP (Subjective, Intervention, Response, and Plan), and PIE (Problem, Intervention, and Evaluation). Each format is tailored to different therapeutic needs and focuses, providing structured guidance that helps clinicians organize their notes efficiently.
Key Features of AutoNotes for Individual Progress Notes:
- Customizable Templates: AutoNotes offers clinicians the flexibility to customize templates according to the specific needs of their individual sessions. Whether it’s adjusting the template to include more detailed assessments or configuring settings to capture client-specific information, AutoNotes adapts to the clinician’s workflow.
- Automated Data Entry: By employing presets that are commonly used in individual sessions across mental health, physical therapy, and occupational therapy, clinicians can quickly populate notes, significantly reducing documentation time. This automation allows clinicians to focus more on the therapeutic process rather than paperwork.
- Enhanced Accuracy and Compliance: With built-in compliance checks, including those required by HIPAA, AutoNotes ensures that all documentation meets the highest standards of accuracy and legality. The platform’s intelligent algorithms help minimize human errors, enhancing the reliability of the individual progress notes.
What is a Progress Note?
A progress note is a critical component of clinical documentation used by healthcare providers to record the details of a patient’s clinical status during a specific encounter. It serves as a continuous log of the patient’s care and is used to track their progress over time. Progress notes are essential for coordinating ongoing treatment, providing a legal record of care, and supporting effective communication among multidisciplinary teams. Typically, these notes include observations, clinical data, treatments administered, and the patient’s response to the treatment, ensuring that all healthcare professionals involved in the care of the patient are informed and aligned in their therapeutic approach.
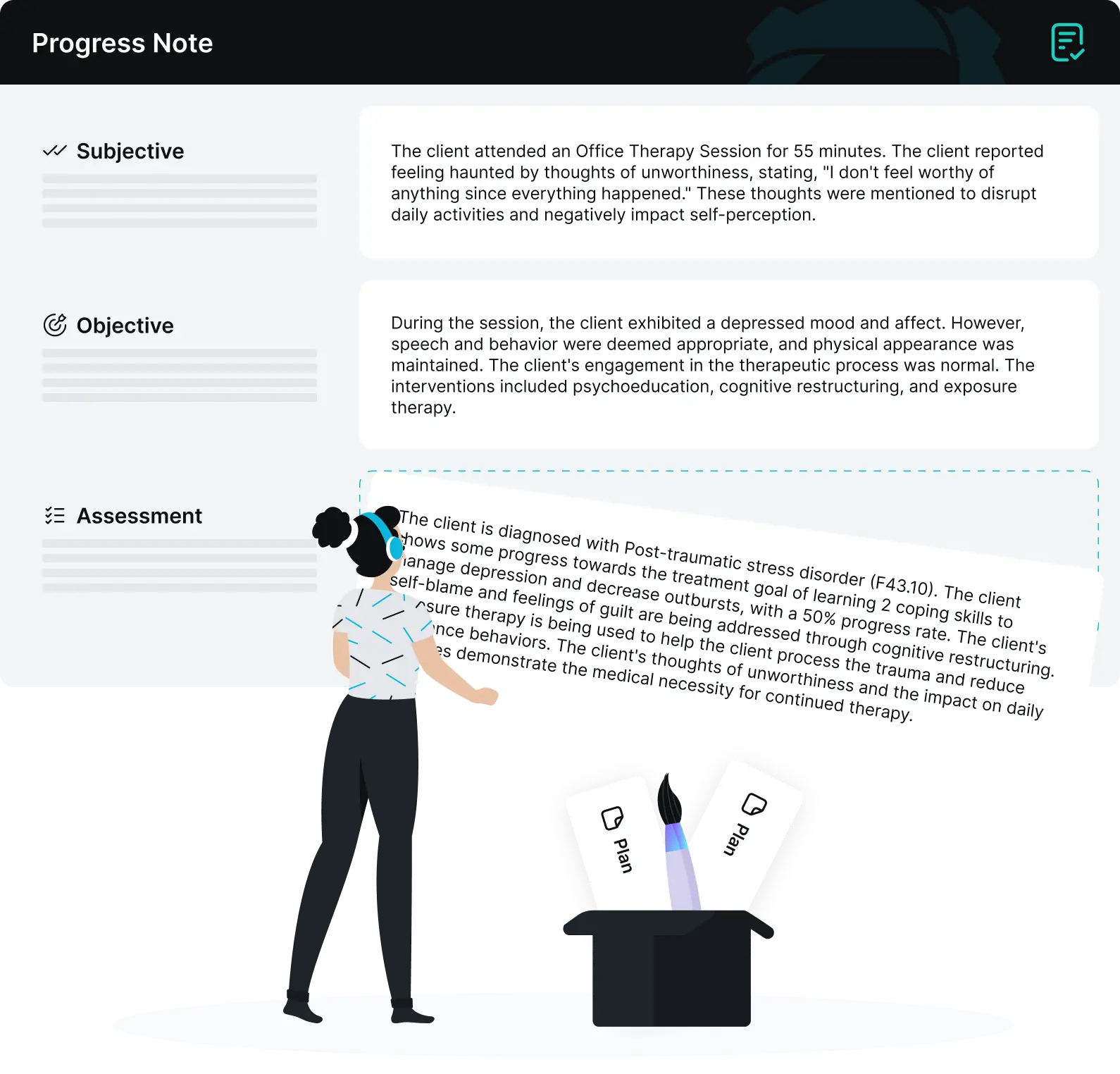
AI Progress Note Example
Below is a hypothetical example of a regular progress note created during an individual therapy session using the SOAP (Subjective, Objective, Assessment, Plan) format. This format helps organize information systematically, enhancing clarity and focus in documentation:
S: Subjective (The patient’s report)
“The patient reports feeling increasingly anxious about upcoming life changes, including a job transition and a move to a new city. They express a persistent worry about adapting to these changes, which has led to difficulty sleeping and concentrating.”
O: Objective (What the clinician observes)
During the session, the patient appeared restless, frequently changing seating positions and fidgeting. Despite reported sleep issues, the patient was alert and engaged throughout the session. No signs of acute distress were observed.
A: Assessment (Clinician’s evaluation and synthesis of the patient’s condition)
The patient’s symptoms are consistent with an adjustment disorder with anxiety. The anxiety level remains moderate but has increased slightly since the last visit, likely due to imminent personal and professional changes. The patient’s willingness to discuss their worries and actively seek coping strategies is a positive indicator of their commitment to managing anxiety.
P: Plan (Next steps for treatment)
- Continue cognitive-behavioral therapy to address anxiety triggers and enhance coping mechanisms.
- Introduce relaxation techniques, including deep breathing and progressive muscle relaxation, to be practiced daily.
- Schedule a follow-up appointment in two weeks to reassess anxiety levels and adjust the treatment plan if necessary.
- Encourage the patient to maintain a regular sleep schedule and limit caffeine intake to improve sleep quality.
This progress note provides a structured summary of the therapy session, addressing both the mental state and the specific needs of the patient. It ensures that any healthcare provider who reads the note will have a clear understanding of the patient’s current condition and the therapeutic approach planned for future sessions.
How to Write a Progress Note with AI in AutoNotes
Writing progress notes in therapy sessions is crucial for tracking client progress and treatment efficacy. AutoNotes, equipped with AI, simplifies this process by providing structured and customizable templates that adapt to various therapy needs. Here’s a detailed guide on using AutoNotes for creating effective progress notes, including both basic and advanced templates.
- Choosing the Right Template: AutoNotes offers two primary types of progress note templates: Basic and Advanced. The Basic template covers essential elements for straightforward cases, while the Advanced template includes more detailed sections for complex cases. Select the template that best fits the session’s needs.
- Customization with Template Settings: Both templates in AutoNotes are customizable using the ‘Template Settings’ feature. This allows therapists to tailor each template according to specific session requirements or client needs, ensuring that all relevant information is captured effectively.
- Documenting Session Information: Start by entering basic session details such as date, time, and duration. AutoNotes structures this information to serve as the foundation for the rest of the progress note.
- Recording Client Interactions and Observations: During the therapy session, significant client interactions and behavioral observations are noted. While AutoNotes helps in organizing these observations, it is vital for the therapist to accurately input detailed and specific descriptions based on their professional observations.
- Assessing Progress: The core of a progress note involves assessing and documenting the client’s progress towards their therapeutic goals. AutoNotes can suggest standardized assessment metrics based on previous entries; however, the therapist must evaluate and decide the most accurate assessments to use, reflecting true progress or challenges faced by the client.
- Intervention Documentation: In this section, document the interventions used during the session. Although AutoNotes provides a structured way to input this information, therapists need to ensure the interventions are described accurately, reflecting the therapeutic strategies employed.
- Evaluating Outcomes and Planning Next Steps: At the end of the session, evaluate the effectiveness of the interventions and plan for future sessions. AutoNotes supports this process with evaluation templates, but the therapist should provide a thoughtful analysis based on the session’s dynamics and outcomes.
- Review and Adjustments: Before finalizing the note, review all the details for accuracy and completeness. AutoNotes allows for easy editing, enabling therapists to make necessary adjustments that best represent the session’s events and discussions.
- Saving and Integrating Notes: Once the progress note is completed, save it within the client’s electronic health records maintained by AutoNotes. This ensures consistency and accessibility for future reference, aiding in ongoing client management and therapeutic continuity.
By utilizing AutoNotes to document progress notes, therapists can efficiently manage their documentation tasks, allowing them to focus more on client interaction and less on paperwork. The customizable templates, combined with AI’s data processing capabilities, ensure that the documentation is not only quick but also precise and reflective of each session’s unique aspects. This approach underscores the therapist’s critical role in evaluating and adjusting the content of the notes to align with professional standards and client-specific therapeutic goals.
The Future of AI in Clinical Documentation
The future of AI in clinical documentation looks promising, with potential advancements in predictive analytics to aid treatment planning and real-time documentation support during sessions. As AI technology evolves, its integration into various therapeutic practices is expected to deepen, offering more sophisticated tools that further enhance the clinician-patient interaction.
Enhancing Healthcare with AutoNotes
The integration of AI in clinical documentation, as exemplified by AutoNotes, represents a significant advancement in healthcare. For clinicians conducting individual sessions, including those in mental health, physical therapy, and occupational therapy, AutoNotes not only simplifies the documentation process but also enhances the accuracy and effectiveness of their notes. As we move forward, the potential for AI to support and transform healthcare practices continues to grow, promising even greater improvements in patient care and treatment outcomes.